Engineered T cells offer a targeted approach to calm overactive immune responses, promising safer and more effective treatments.
Scientists at UC San Francisco have developed a groundbreaking way to treat autoimmune diseases and improve outcomes for organ transplant patients. They’ve engineered special immune cells, called T cells, that act as “peacemakers” in the body. These cells calm down overactive immune responses and reduce harmful inflammation without the need for strong immune-suppressing drugs. Current treatments often leave patients more vulnerable to infections and other complications, but this new method could avoid those risks.
One major application for these engineered cells is to prevent the rejection of transplanted organs or tissues, such as the pancreatic islet cells used to treat type 1 diabetes. Patients receiving these transplants currently rely on powerful drugs to stop their immune systems from attacking the new tissue. While effective at preventing rejection, these drugs have many side effects, like increased susceptibility to infections and a higher risk of other illnesses. The new technology offers a more precise approach. It helps the immune system accept transplanted tissues while still protecting the body from infections and cancer.
To create these cells, the researchers were inspired by the body’s natural “suppressor” cells, which act like brakes on the immune system to prevent it from overreacting. However, in conditions like type 1 diabetes, these natural brakes often don’t work well enough. To address this, the scientists engineered CD4 T cells (a type of immune cell already used in some cancer therapies) to take on suppressor roles. They also equipped these cells with special sensors so they can find and work in specific areas of the body where they’re needed most.
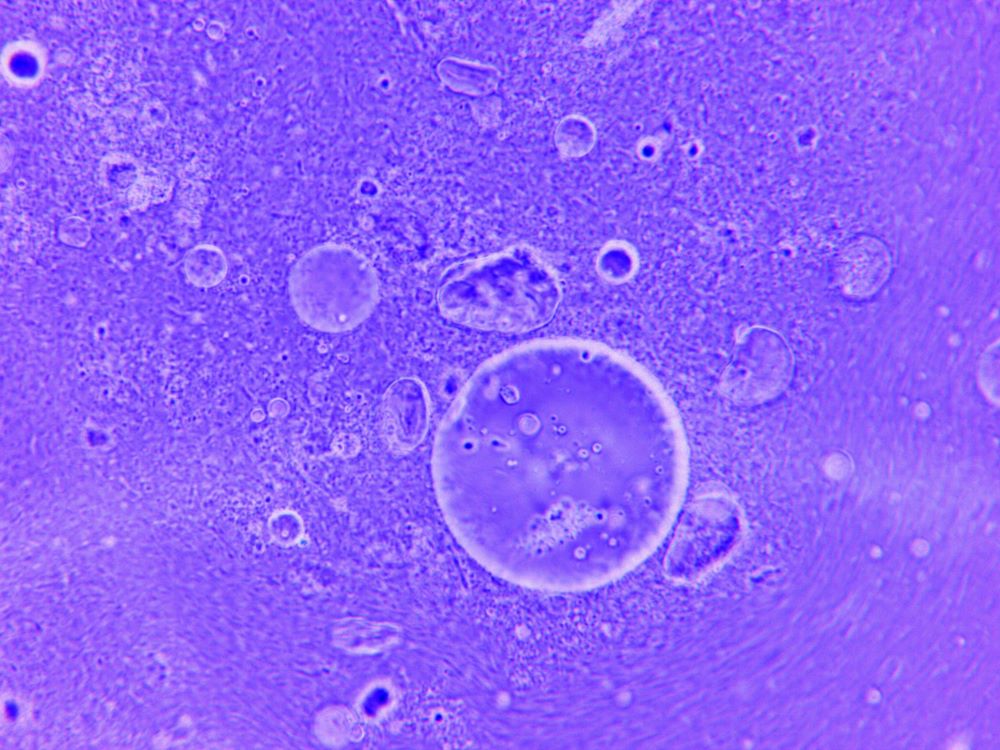
In an experimental model, the engineered cells were designed to recognize and protect human pancreatic islet cells. These cells are critical for producing insulin, which regulates blood sugar levels. When tested in mice with transplanted islet cells, the engineered cells successfully stopped the immune system from attacking the transplant. As a result, the transplanted tissues survived and functioned properly. This early success suggests that, in the future, people with type 1 diabetes could receive islet cell transplants without needing lifelong immune-suppressing drugs or daily insulin therapy.
Beyond type 1 diabetes, the scientists believe their engineered cells could be used to treat a wide range of autoimmune diseases and improve outcomes for organ transplants. Unlike current treatments that suppress the entire immune system, this approach targets the specific areas where the immune system is malfunctioning. By restoring balance in localized tissues, the therapy reduces side effects and improves safety for patients.
The potential applications don’t stop there. The researchers think this technology could also make cancer treatments safer and more effective. For example, CAR T cell therapy, a method that modifies immune cells to attack cancer, can sometimes harm healthy tissues along with the cancerous ones. By adding the same precision features to CAR T cells, the therapy could better distinguish between cancer cells and healthy cells, reducing collateral damage.
This new approach could significantly benefit people with autoimmune diseases, cancer, or transplant needs. Autoimmune diseases are notoriously difficult to treat because they involve the immune system attacking the body’s own tissues. With these engineered cells, doctors could address these conditions more precisely, improving patient outcomes without compromising overall health. Similarly, transplant patients could avoid the long-term risks associated with current immunosuppressive drugs, and cancer patients could receive more targeted and less toxic treatments.
In addition to being safer, this technology represents a step toward personalized medicine. Instead of using one-size-fits-all treatments, doctors could tailor therapies to each patient’s specific condition. For example, engineered cells could be programmed to focus on the unique immune dysfunction in a patient’s body, whether it’s in the pancreas, kidneys, or another organ. This personalized approach could help patients not only survive but also enjoy a better quality of life.
Sources:
Engineered immune cells could transform treatment for autoimmune diseases
Engineering synthetic suppressor T cells that execute locally targeted immunoprotective programs


Join the conversation!