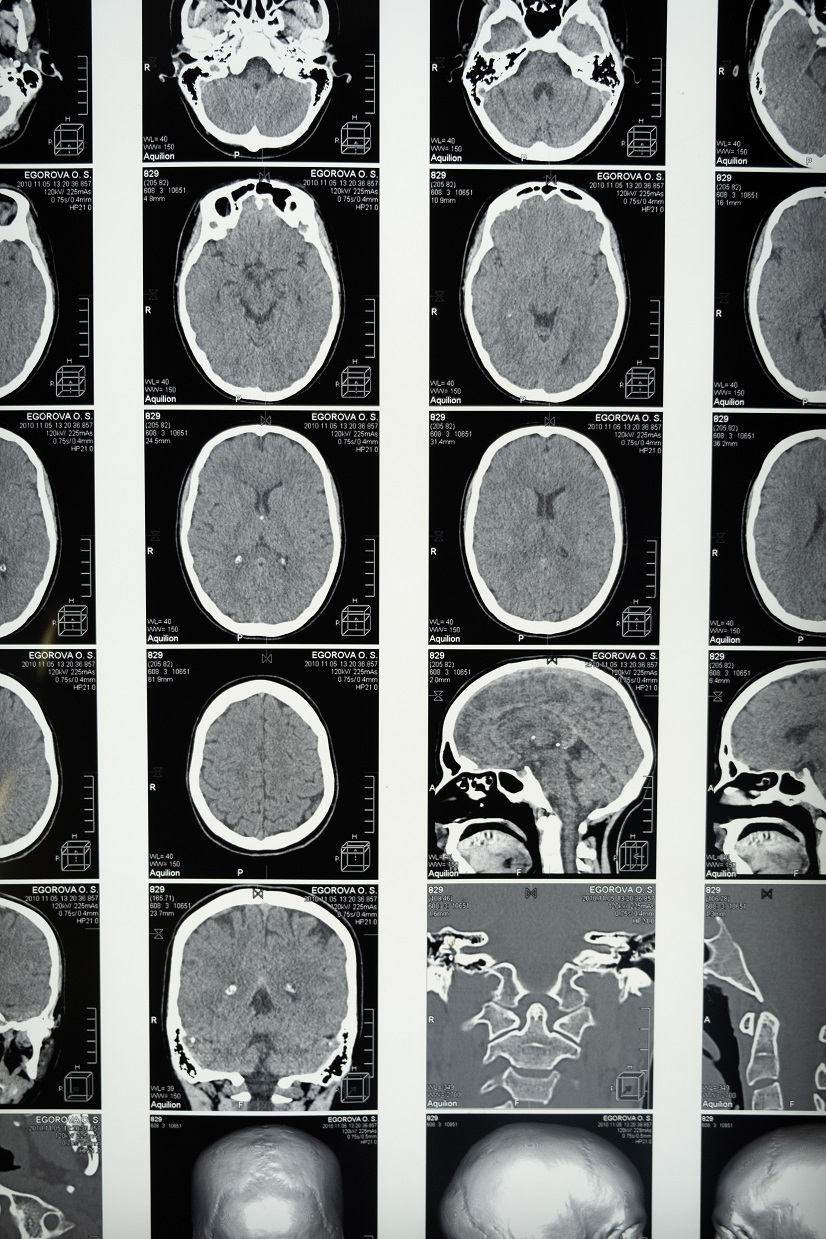
Studies have shown the coronavirus can have a permanent impact on the brain.
The coronavirus impacts the brain – big time. And research shows this is what’s happening even during mild COVID cases when patients lose their sense of smell. In early studies, the loss of smell alone seemed to be, in and of itself, an adequate-enough sign that an individual has contracted the novel virus. Furthermore, it was a sufficient predictor that the upper respiratory distress a patient was presenting with was caused by COVID. Contrary to an early belief that the loss of smell would be temporary and pass when a patient no longer tested positive, many people have reported prolonged lacking this sense even long after the infection has run its course. Thus, researchers became determined to find the reasoning behind lingering symptoms, and it is now known that the nervous system is impacted. Brain damage can occur.

Late last month, an article published in JAMA Network Open, sought to use data from spinal taps to determine exactly how the brain is affected. The virus is commonly known to cause brain fog, extreme fatigue and problems with concentration and memory. These issues are linked to what has been coined “long COVID.” COVID can cause brain damage and subsequent neuropathy and delirium.
Scientists collected data from the UK Biobank database, “looking at brain magnetic resonance imaging (MRI) scans and tests of brain function in 785 volunteers.” They discovered, “About half of those participants had mild COVID infection, and the other half had contracted the virus. This allowed the team to determine the effects of mild COVID infection on brain structure and function.” In doing so, the team found that those with only a mild infection experienced some brain shrinkage.
The team also reported, “Among those that had not experienced neurological complications while hospitalized, 88% reported new cognitive symptoms. These cognitive impairments seem to be separate and apart from damage due to hypoxia, or the lack of oxygen to the brain, often experienced by those hospitalized for severe COVID-19.”
To build upon these initial findings, which were published in March in the journal Nature, Arvid Edén, from Sweden, and his colleague examined the cerebrospinal fluid of patients hospitalized with COVID. Twenty-one patients with the virus and nervous system pathology (mostly encephalopathy), 23 patients with COVID and no nervous system problems, 41 hospitalized patients without COVID, and 10 healthy controls were all part of the study.
They found, “Of 44 patients with COVID-19 (23 neurosymptomatic) included in this hospital-based cross-sectional study, CSF nucleocapsid antigen was detectable in 89% of patients with available data and was significantly correlated with immune activation markers (neopterin and interferon γ). Moreover, neurosymptomatic patients had a more pronounced inflammatory CSF profile compared with neuroasymptomatic patients that could not be attributed to differences in COVID-19 severity.”
In other words, no matter the severity of symptoms when one contracts the coronavirus, the brain is at risk of impairment.
Sources:
This Is Your Brain on COVID-19
SARS-CoV-2 is associated with changes in brain structure in UK Biobank
Even mild COVID can cause brain shrinkage and affect mental function, new study shows

Join the conversation!