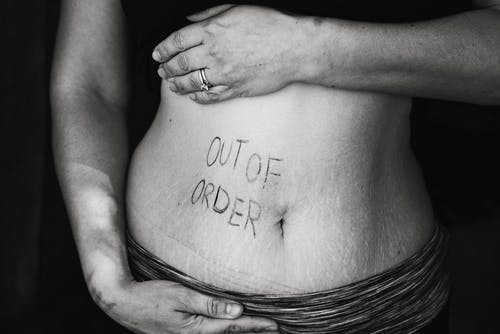
Researchers find NFEPP treatment for irritable bowel does not come with adverse effects.
According to new research published in the journal Gut, a targeted opioid, NFEPP, that only treats diseased tissues and spares healthy tissues can relieve pain from inflammatory bowel disease. The study, led by researchers at New York University College of Dentistry and Queen’s University in Ontario, was conducted in mice with colitis, and it was discovered that the opioid treated symptoms without adverse effects.
The types of inflammatory bowel disease include ulcerative colitis, a condition involving inflammation and ulcers along the lining of the large intestine (colon) and rectum, and Crohn’s disease, involving the inflammation of the lining of the digestive tract. Opioids relieve pain by targeting opioid receptors, including the mu opioid receptor.
“We wanted to understand whether it is possible to activate this receptor only in diseased tissues and not in normal tissues,” said senior study author Nigel Bunnett, PhD, professor and chair of the Department of Molecular Pathobiology at NYU College of Dentistry. “Essentially, can you control pain without triggering these devastating side effects?”

And the team found that NFEPP, discovered by Christoph Stein, MD, of Charité-Universitätsmedizin Berlin, a collaborator on the Gut study, may be the solution. NFEPP is a reengineered form fentanyl with an added fluorine atom that only binds to the mu opioid receptor in an acidic environment. In lab tests, both NFEPP and fentanyl inhibited colon pain in mice with colitis. Yet, unlike fentanyl, NFEPP did not cause side effects.
“Whereas fentanyl decreased defecation and caused respiratory depression and hyperactivity in mice with colitis, NFEPP was devoid of these effects,” the authors write, concluding, “In a preclinical IBD model, NFEPP preferentially activates MOPr in acidified microenvironments of inflamed tissues to induce anti-nociception without causing respiratory depression, constipation and hyperactivity.”
“The preference of NFEPP for activating opioid receptors in acidic tissues accounts for its ability to selectivity relieve pain in the inflamed but not healthy colon,” said Bunnett. “By sparing healthy tissues, we avoided the detrimental side effects seen with fentanyl use.”
The next steps will be to test NFEPP’s ability to inhibit pain in the human gut and ultimately conduct clinical trials.
“Treatments designed to preferentially engage opioid receptors in diseased tissues could offer the potential for effective pain relief without the side effects. These drugs would represent a major advance in the treatment of painful diseases, including inflammatory bowel disease and cancer,” said Bunnett. “More broadly, engineering drugs beyond pain treatments that target only diseased tissues could open the door to more effective and precise therapies for a wide range of disorders.”
In addition to Bunnett, the study’s authors are Nestor Jimenez-Vargas and Yang Yu of Queen’s University and Dane Jensen of NYU College of Dentistry and Stephen Vanner of Queen’s University. Collaborators are from Queen’s University, NYU College of Dentistry, Columbia University, and Charité-Universitätsmedizin Berlin. The research was supported by grants from the National Institutes of Health and the U.S. Department of Defense, Crohn’s Colitis Canada, and Deutsche Forschungsgemeinschaft.
Sources:
Inflammatory bowel disease (IBD)
Study in Mice Points to Promising Treatment for Pain in Inflammatory Bowel Disease

Join the conversation!