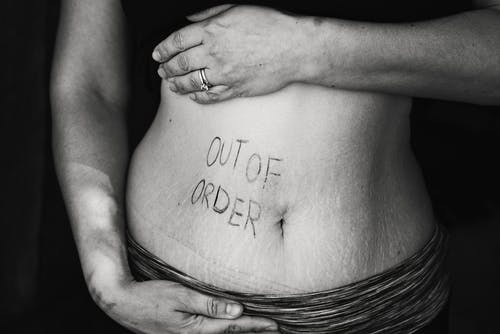
The gut has a big impact on mental health, according to researchers.
Enteroendocrine cells are those found within the gastrointestinal tract, stomach and pancreas (essentially the “gut” region) that produce hormones to control how our food is taken in and digested. When these cells are compromised the gut flora can be thrown off, which can lead to a whole host of gastrointestinal issues, including indigestion, vomiting, and a “sore tummy.” Now research has shown that not only will imbalanced enteroendocrine cells cause poor gut health but this could also impact the brain.
The gut-brain connection has been known and studied for some time. It connects the central nervous system (CNS) and gastrointestinal tract, which work together to help maintain body balance and help an individual feel well. Otherwise, people begin to feel sick and when this happens, the brain begins to feel sick.

In a recent paper published online last year iin the Chinese Medical Journal, a research team led by Dr. Yong-Zhan Nie analyzed studies focused on the interactions between gut hormones and microbiota and emphasized their role in the development of both physiological and psychological gut-brain axis mental health disorders. For the most part these disorders can be alleviated with a well-balanced diet. However, some are permanent, if the damage is extensive enough.
As Dr. Nie explains, “Modern tools like sequencing technology and bioinformatics have opened new doors to the elusive world of microbiology and neuroscience, leading to some fascinating research exploring the effect our gut microbiology has on our brain. Our aim was to bring such original studies and reviews under one roof.”
The study suggests that “microbiota and the related hormones also influence the development of digestive conditions like metabolic disturbances and inflammation disorders. Recent studies show that hormones in the gut-brain axis may even link back to neurological and psychological disorders.”
Harvard Health has previously suggested, “Given how closely the gut and brain interact, it becomes easier to understand why you might feel nauseated before giving a presentation or feel intestinal pain during times of stress. That doesn’t mean, however, that functional gastrointestinal conditions are imagined or ‘all in your head.’”
Poor psychology also causes issues to the gut to become impaired, and compromises the way the body physically handles stress. For example, anxiety, stress or depression, among other factors, can affect bowel movements and contractions of the GI tract. Neurological disorders like epilepsy, autism, and Parkinson’s disease.
“Gut hormones that relay hunger signals to the CNS often play a crucial role in the development of mood disorders and obesity. For instance, ghrelin, a neuroactive gut hormone that activates food craving, also regulates stress response, depression, and anxiety. Studies show that a reduction in ghrelin concentration in our body reduces anxiety levels and also the urge to eat high-calorie foods,” according to the new study. This can help one live a healthier lifestyle.
“Our overview can help scientists further explore the relationship between microbiota-hormones-gut brain axis and develop novel therapeutics for different psychiatric and gastrointestinal disorders, such as obesity, anxiety, and depression,” concludes Dr. Nie.

Join the conversation!